Wednesday, November 19, 2008
Saturday, November 15, 2008
Toxoplasmosis awareness, causes and prevention
 Toxoplasmosis (toxo) is an infection caused by a single-celled parasite called Toxoplasma gondii .The infection is most commonly acquired from contact with cats and their feces or with raw or undercooked meat.
Toxoplasmosis (toxo) is an infection caused by a single-celled parasite called Toxoplasma gondii .The infection is most commonly acquired from contact with cats and their feces or with raw or undercooked meat.The U.S. Centers for Disease Control and Prevention (CDC) estimates that more than 60 million people in the United States may carry the Toxoplasma parasite, but very few have symptoms because a healthy immune system usually keeps the parasite from causing illness.
 What factors increase the risk of acquiring toxo?
What factors increase the risk of acquiring toxo?The following situations potentially expose a person to the toxoplasma parasite and increase the risk of acquiring toxoplasmosis:
touching your hands to your mouth after gardening, cleaning a cat's litter box, or anything that came into contact with cat feces
eating raw or partly cooked meat, especially pork, lamb, or venison
touching your hands to your mouth after contact with raw or undercooked meat
organ transplantation or transfusion (this is rare)
If a woman is pregnant when she is infected with toxo, the infection can be transmitted from her to the baby with sometimes catastrophic consequences.
What are the usual symptoms of toxoplasmosis?
Although people infected with toxoplasmosis are often unaware of having this disease, typical symptoms of toxo are flue like symptoms including swollen lymph nodes and muscle aches and pains that last from a few days to several weeks. If your immune system is normal, you cannot get the infection again.
Why do some people develop severe problems from toxo?
Few people with toxo develop symptoms because the immune system usually keeps the parasite from causing illness. However, anyone with a compromised immune system is at risk for serious problems from toxo. These individuals include those undergoing chemotherapy, people with HIV/AIDS or other immune disorders, and recent organ-transplant recipients.
In these people, an infection that occurred anytime during life can reactivate and cause the severe symptoms of toxoplasmosis such as damage to the eye, brain, or other organs.
Ocular toxoplasmosis, which damages the eyes, can lead to reduced vision, blurred vision, pain (often with bright light), redness of the eye, and sometimes tearing, according to the CDC.
Can toxoplasmosis develop into a more serious illness in babies?
Yes, the immune system in infants is not fully mature until after birth.
The babies of women who were exposed to toxo within a few months of becoming pregnant or during pregnancy are at an increased risk for developing a severe case of toxo. According to the NIH (U.S. National Institutes of Health), pregnant women who newly contract the toxoplasmosis parasite have a 40% chance of transmitting it to their unborn child. Women who were first exposed to toxo more than six months before becoming pregnant are not likely to pass the infection to their children.
Most infants have no symptoms at birth, but a small percentage may be born with eye or brain damage. Unfortunately, the signs and symptoms of the disease often appear a few months after birth.

What is meant by a baby developing "a more severe case of toxo"?
Children born with toxoplasmosis can be afflicted with mental retardation, convulsions, spasticity, cerebral palsy, deafness, and severely impaired vision. The infant's head may be abnormally small (microcephaly) or abnormally large due to increased pressure on the brain (hydrocephalus).
How is toxo diagnosed in the lab?
There are many different kinds of blood tests for toxoplasmosis. The results can determine if the patient has had toxo and whether the infection is recent ("acute") or not.
How can toxoplasmosis be prevented?
Since toxo usually causes mild to no symptoms, and a healthy immune system prevents any remaining parasites in the body from causing further symptoms, most people don't need to worry about getting this disease.
However, if you have a weakened immune system or are pregnant, there are several steps you should take to prevent exposure to toxoplasmosis.
If you have a weakened immune system, get a blood test for toxoplasmosis. If your test is positive, your doctor can tell you if and when you need to take medicine to prevent the infection from reactivating.
If you are planning on becoming pregnant, you may consider being tested for toxo. If the test is positive, there is no need to worry about passing the infection to your baby (since you should have immunity against the parasite).
If you are already pregnant, you should discuss your risk of toxoplasmosis with your doctor who may order a blood sample for testing.
Wear gloves when you garden or do anything outdoors that involves handling soil since cats often use gardens and sandboxes as litter boxes. Wash your hands well with soap and warm water after outdoor activities, especially before you eat or prepare food.
Have someone else handle raw meat for you. If this is not possible, wear clean latex gloves and thoroughly wash with soap and hot water any cutting boards, sinks, knives, and other utensils that might have touched the raw meat. Wash your hands well with soap and warm water afterward.
Cook all meat thoroughly, especially pork or veal.

Yes, but if you have a weakened immune system or are pregnant, there are some steps to take to avoid being exposed to toxo according to the Cornell College of Veterinary Medicine.
Most importantly, you can help prevent your cats from getting infected with toxo. Feed them dry or canned cat food and keep them indoors. Cats can become infected by eating or being fed raw or undercooked meat that is infected with the parasite, or by eating infected prey such as birds or rodents. Any cat that is allowed access to outdoors should be kept off beds, pillows, or other furniture that you also use. Don't bring a new cat into your house that might have been an outdoor cat or might have been fed raw meat. Avoid handling stray cats and kittens. Have your cat tested for the parasite. Your vet can answer any other questions you may have regarding your cat and the risk for toxoplasmosis.
Have someone who is healthy and not pregnant change your cat's litter box. If this is not possible, wear gloves and clean the litter box daily (the parasite found in cat feces needs a few days after being passed to become infectious). Wash your hands well with soap and warm water afterward.
Once infected with toxo, is my cat always able to spread the infection to me?
No, cats can only spread toxo in their feces for a few weeks after they are first infected with the parasite. Like humans, cats rarely have symptoms when first infected, so most people don't know if their cat has been exposed to toxo. In fact, most infected cats appear healthy. There are no good tests available to determine if your cat is passing toxo in its feces.
What is the treatment for toxoplasmosis?
Once the diagnosis of toxoplasmosis is confirmed, you and your doctor should discuss whether treatment is necessary. In an otherwise healthy person who is not pregnant, treatment is not needed. Symptoms will usually go away within a few weeks. For pregnant women or people who have weakened immune systems, drugs are available to treat the parasite that causes toxoplasmosis.
Toxoplasmosis At A Glance
· Toxoplasmosis (toxo) is a disease caused by a parasite.
· Toxo is acquired from contact with cats and their feces.
· Toxo is also acquired from eating or touching raw or partly cooked meat.
· Symptoms can range from none to very severe.
· A woman who contracts toxo right before or during pregnancy can transmit it to her baby with catastrophic consequences.
· People with immune deficiencies are at high risk for developing severe signs and symptoms of toxo.
Featured:
Toxoplasmosis (toxo) is a parasitic infection that causes flulike symptoms, swollen lymph nodes, and muscle aches and pains that may last from a few days to several weeks. Pregnant women who contract toxo have a 40% chance of passing the infection to their babies. Babies born with toxo may be afflicted with mental retardation, cerebral palsy, deafness, and severely impaired vision.
Medication for Toxoplasmosis
GENERIC NAME: PYRIMETHAMINE - ORAL (pir-ih-METH-uh-meen)
BRAND NAME(S): Daraprim
USES: This medication is used in the treatment and prevention of prevention of malaria or the treatment of Toxoplasmosis (a parasitic infection). Pyrimethamine is often taken in combination with other antimalaria medication.
HOW TO USE: Take this medication by mouth with food or meals as directed. For preventing malaria, this is usually taken once a week. For treatment of a malarial attack, this is taken once a day for 2 days, then given once a week. In the treatment of toxoplasmosis, this may be given once or twice a day for up to 5 weeks. Take this medication for the full time prescribed. Stopping therapy too soon may result in ineffective treatment.
SIDE EFFECTS: Nausea, stomach upset or loss of appetite may occur especially the first several days as your body adjusts to the medication. Other effects reported include headache, lightheadedness, dry mouth, diarrhea, trouble sleeping. If any of these effects continue or become bothersome, inform your doctor. Notify your doctor if you develop a sore throat, unusual bruising, pale skin, swelling of the tongue, depression, irregular heartbeat. Use caution driving or operating machinery if this medication makes you lightheaded. This medication may cause blood disorders. It is important that lab tests be done periodically while taking this medication to monitor for this. A serious allergic reaction to this drug is unlikely, but seek immediate medical attention if it occurs. Symptoms of a serious allergic reaction include: rash, itching, swelling, dizziness, trouble breathing. If you notice other effects not listed above, contact your doctor or pharmacist.

A is for animals, Z is for zoonoses.
They come from giant Gambian rats and fuzzy bunnies. They come from puppies and pythons. Whether the animal is friend or food or foe, it can carry dangerous diseases.
There are at least 39 important diseases people catch directly from animals. There are at least 48 important diseases people get from the bite of bugs that bit an infected animal. And there are at least 42 important diseases that people get by ingesting or handling food or water contaminated with animal feces.
Some are as old as memory: rabies, bubonic plague, food poisoning. Others have only recently emerged: monkeypox, West Nile encephalitis, Legionnaires' disease. And some, such as highly lethal bird flu, we fear even though they haven't -- yet -- spread in humans.
People have lived with animals for eons. There's a reason for that. They don't just make us feel better. They actually contribute to our health. People who keep pets tend to have lower cholesterol levels and lower blood pressure. They tend to get more exercise and to feel less lonely.
On the other hand, pets and other animals can get sick. And some of these illnesses can be quite dangerous. This article offers an overview of these diseases -- and how to avoid them.
Why Animal-Borne Diseases Matter
Diseases passed to humans from animals are called zoonoses. What makes one of these diseases important? Two things, "If you ask Americans in general what is the most important zoonosis, most would say rabies," "It is something they fear, it is in the news. But in terms of risk, there are only zero to two human cases a year in the U.S. It's one of those zoonoses that are important because of their seriousness, but not their frequency: rabies, tularemia, plague, monkeypox, listeria, anthrax. These are diseases that are very serious if one gets them but which are relatively uncommon."
On the flip side, are animal-borne diseases that are important because they are fairly common even if not often fatal. Cat-scratch fever, for example, infects as many as 20,000 Americans a year. And an estimated 4%-20% of U.S. kids get roundworm from dogs and cats.
 Toxoplasmosis
ToxoplasmosisCats allowed to roam outdoors often pick up a parasite known as Toxoplasma gondii. Most of the time, the cat will fight off the infection before it becomes contagious. However, sometimes cats shed egg-like forms of the parasite in their feces. That's why pregnant women, small children, people with damaged immune systems, and people on cancer chemotherapy should avoid cleaning cat litter boxes.
Usually, a person who gets toxoplasmosis gets very few symptoms. But when a person does get the disease, it causes a flu-like illness and/or muscle aches and pains lasting for a month or even longer. "A very sizeable proportion of humans -- 30%-40% -- have been infected with toxoplasmosis, usually by eating undercooked meat," Glickman says. "Most people never had a symptom or had very mild disease. But in people [with weakened immune systems] it can be fatal. And the worst infections may be in pregnant women. The organism can go to the fetus and, if the baby doesn't die, cause lifetime illness."
Diseases from Cats and Dogs
By far they're our best friends. And that means cats and dogs are common sources of disease.
Cats often carry a germ called Bartonella henselae. Some 40% of cats are infected at least once in their lives -- usually when they're kittens -- but they don't look sick. Humans get infected only when they are bitten or scratched by an infected animal -- cat-scratch fever

Other bacterial infections humans can get from cats and dogs include:
Plague. Rodents carry the plague bacteria. Very rarely, cats get fleas from infected rodents and pass the disease to humans.
Q fever.
People are much more likely to get Q fever from barnyard animals than from cats. But it does happen. Half of infected people get symptoms that include fever, headache, chest or stomach pain, diarrhea, and/or vomiting. It can also cause temporary swelling of the heart -- a dangerous event for people who already have heart disease.
Campylobacter infection. Found in animal feces, this germ causes gastrointestinal symptoms. It's usually not dangerous, but can cause severe illness in people with weakened immune systems.
Leptospira infection.
Humans get infected via contact with water, food, or soil containing urine from infected animals. Left untreated, leptospirosis can be quite serious. It can lead to liver failure, trouble breathing, kidney damage, brain and spinal cord infection, and, rarely, death. Symptoms vary widely but can include high fever, severe headache, chills, muscle aches, and vomiting. There may also be yellow skin and eyes, red eyes, abdominal pain, diarrhea, or a rash.
Salmonella
infection. People get this often-severe gastrointestinal infection via contact with animal feces. It can cause severe kidney damage to young children.
Both cats and dogs sometimes get parasites that infect humans. One of the most common is roundworm. Left untreated, nearly all puppies and kittens pick up this parasite. Its egg-like form -- the oocyst -- can survive for years in soil.
When humans ingest oocysts, tiny worms hatch in the gut and move through the body. Symptoms include fever, coughing, asthma, and/or pneumonia. Once in a while, the tiny worms enter the eye and scar the retina. This results in permanent partial vision loss. "Some 750 to 1,500 kids go blind each year with roundworm infection [of the eyes] passed from dogs through feces to children.
Other parasites of cats and dogs:
 Tapeworm.
Tapeworm. A person gets infected by swallowing an infected flea -- a relatively rare event, but it happens.
Hookworm. Hookworms are common in tropical and subtropical areas. They infest soil contaminated by animal feces. Humans get infected by direct contact, usually by walking on contaminated soil. Heavy infections can be serious.
Cryptosporidiosis.
This parasite cause mild to severe intestinal symptoms like diarrhea. It's not usually a dangerous infection, except to people with weakened immune systems.
Ringworm
isn't a parasite, but a fungal infection that forms a ring-shaped rash on the skin or a bald patch on the scalp. People can get it from direct contact with an infected animal.
Cats and dogs get viruses, too. Rabies is the most dangerous one. Be sure to keep up with your pet's rabies vaccination.
To protect yourself from diseases carried by house pets:
· Wash your hands with soap and running water after touching feces.
· Take your pet to the vet on a regular basis and keep up with all vaccinations recommended for your area.
· Avoid rough play with cats.
· If your cat or dog bites you, wash the area with soap and water right away.
· Wash your hands after handling your pet -- especially before eating or preparing food.
· People with weakened immune systems should take special precautions. These include never letting pets lick them on the face or on an open cut or wound, never touching animal feces, and never handling an animal that has diarrhea.
· Don't let your pet drink from toilet bowls or eat feces.
 Other Pets, Other Diseases
Other Pets, Other DiseasesWe humans have other friends besides cats and dogs. And with these other friends come other diseases:
Birds. Pet birds, including parrots and parakeets, can spread psittacosis. It's a relatively rare disease, with about 50 U.S. cases each year. Symptoms include fever, chills, headache, muscle aches, and a dry cough. There's often pneumonia, which can be quite serious and even fatal. Untreated infections can lead to serious heart, liver, and nerve problems.
Reptiles and amphibians. Snakes, turtles, lizards, frogs, toads, and salamanders -- like other animals -- can carry Salmonella bacteria. Wash your hands after handling them. Keep them in their habitat; don't let them wander your room. Keep reptiles and their equipment away from the kitchen. Don't clean reptile cages in sinks or tubs used by people. Don't kiss your reptile -- it won't like it, anyway. And keep reptiles and amphibians away from children younger than 1 and people with weakened immune systems.
Exotic animals. Yes, some people make pets of animals like African pygmy hedgehogs. These tiny, antisocial animals that roll up into spiky balls were a fad not too long ago. And they came with salmonella. More recently, pet Gambian giant rats brought monkeypox into the U.S. Similar to smallpox -- but fortunately milder and not as contagious -- monkeypox lurks in small mammals in the African rainforest.
Wild Animals
Wild animals should stay that way. Enjoy them from a distance. Even so, they're a rich source of human disease. Here are a few:
Raccoon roundworm.
This is the best reason not to feed wild racc
 oons. The feces of an infected raccoon carry millions of roundworm eggs. These eggs become infectious in two to four weeks and can survive for years in the environment. They are very difficult to kill -- the CDC recommends cleaning contaminated decks or porches with boiling water or a propane flame gun (with proper caution, of course).
oons. The feces of an infected raccoon carry millions of roundworm eggs. These eggs become infectious in two to four weeks and can survive for years in the environment. They are very difficult to kill -- the CDC recommends cleaning contaminated decks or porches with boiling water or a propane flame gun (with proper caution, of course).Symptoms depend on where the roundworms travel in the body. They can include nausea, fatigue, enlarged liver, and symptoms of brain infection (poor coordination, inattention to one's surroundings, loss of muscle control, coma, and/or blindness). Some infections have been fatal. Diagnosis is difficult. If you are having symptoms after contact with raccoons, be sure to tell your doctor. There is no specific cure, but early treatment can limit the extent of disease.
Giardia infection. This microscopic parasite is the hiker's bane. It's one of the main reasons why you should always purify water taken from a stream, no matter how far from civilization you're camping. An infected animal sheds Giardia in its feces. It can survive for a long time in water and in soil.
 Symptoms include, loose or watery diarrhea, stomach cramps, and stomach upset. People with Giardia infection are contagious and easily spread the parasite to others. Fortunately, there are excellent curative treatments.
Symptoms include, loose or watery diarrhea, stomach cramps, and stomach upset. People with Giardia infection are contagious and easily spread the parasite to others. Fortunately, there are excellent curative treatments.Hantavirus.
Lymphocytic choriomeningitis (LCM).
This is a virus spread by the common house mouse. The virus can infect the linings of the brain and spinal cord. It's a serious disease, although many people get only mild infections. Mice shed the virus in their urine, saliva, and feces. People get infected by eating contaminated food or by inhaling aerosolized mouse urine or feces. LCM has two phases. The first lasts about a week and begins with fever, loss of appetite, head and muscle aches, nausea, and/or vomiting. There may be other symptoms as well. The second phase happens just as the first one gets better. It may begin with symptoms of meningitis: fever, headache, and stiff neck. It may also begin with symptoms of encephalitis: sleepiness, confusion, and movement problems. There's no cure, but most people recover completely with supportive treatment. However, some people are left with permanent nerve or brain damage. About 1% of people with LCM die.
 Tularemia (rabbit fever).
Tularemia (rabbit fever). People usually get tularemia from direct contact with rabbits. A person can also get it via the bite of an infected tick or deerfly, by eating contaminated food, by drinking contaminated water, or by breathing in F. tularensis, the bacteria that causes rabbit fever. It's very infectious: Fewer than 10 microscopic germs can cause a lethal infection. This is why tularemia was studied during World War II as a germ warfare agent. The kind of disease one gets depends on how one is infected. The inhaled form is most severe, with a 30%-60% fatality rate in untreated cases. It causes pneumonia with sudden fever, chills, muscle and joint aches, dry cough, and progressive weakness. In severe cases there is bloody spit with difficulty breathing.
Equine Encephalitis and West Nile Viruses
The equine encephalitis and West Nile viruses are transmitted from wild birds to humans -- and to horses -- by mosquitoes. It can cause a very dangerous infection of the brain and spinal cord. So can equine encephalitis, which has long been firmly rooted in the U.S. In fact, eastern equine encephalitis is considered a much more serious disease. About 30% of people who get it die, and another 30% have lasting nerve damage.
Most years there are very few cases of equine encephalitis. But some years are much worse than others -- and there's no way to predict in advance when there will be an outbreak.
Ebola Virus
It's hard to think of a more horrible disease than Ebola hemorrhagic fever. Ebola virus is spread by contact with the blood or body fluids of an infected person. Does it come from animals? Probably. Monkeys and great apes get it -- and people can get it from them when they butcher them for food. But monkeys die of Ebola, so they can't be the ultimate host. Most researchers think there's an animal out there harboring the virus. They just haven't found it yet.
 SARS
SARSThat SARS emerged in China's Guangdong province seems sure. What's not sure is where it came from. SARS is a coronavirus, but it's not like any other member of the coronavirus family. Some researchers think it may have come from an endangered animal known as a masked palm civet -- like most exotic animals, a culinary delicacy in parts of China. Others find the evidence weak. Whether SARS evolved in animals or humans remains a matter of debate.
Influenza, bird flu viruses
One disease that's definitely evolving in animals is influenza. And one place it's evolving is none other than Guangdong, China, where animals are kept in close proximity to one another. Flu viruses tend to arise in ducks and geese. They spread to chickens and to pigs. Pigs can also get infected with human flu viruses, so they make a good mixing pot for new flu. When an animal or a person is infected with two different flu viruses, the viruses like to swap parts. Voilà! A new virus emerges.
Infectious disease specialists don't wonder whether there will be a new worldwide flu epidemic. They only wonder when it will happen. There have been two recent close calls.
In 1997, lethal bird flu arose in the poultry markets of Hong Kong. People got infected and died, but the slaughter of millions of chickens stopped the virus before it learned how to spread from person to person. In 2001 and 2002, similarly bird flu viruses evolved in Hong Kong chickens. Fortunately, they didn't spread to humans.
What Puts Us At Risk?Animals can pass parasites on to humans. Children should not kiss or be kissed or licked by pets. This is a very easy pathway for parasites to enter the human body. Keep infants and toddlers away from pets that have not been wormed.
Hands should be washed after each and every contact with a pet, otherwise one is putting self at serious risk.
Animals that are strictly indoor animals and that do not come into contact with the outdoors are a much lesser risk, but still a risk. Animals that come and go from the outdoors into the home pose a serious risk, especially to children. Cats and dogs for example clean their anus with their tongues. If they lick you, they are transferring parasites to your skin. If they lick your face, it does not take long for the parasite to find its way into your mouth and your intestine.
Toxoplasmosis and is usually acquired from cats. A small scratch from a cat or dog can also transmit the parasite. Cats use a cat box. They are moving around feces and urine that has been prior deposited in the cat box. This dirt that has parasites.
Cat boxes should be scooped daily and thoroughly bleached and washed on a weekly basis.
Make sure you use gloves; put two pair on when doing this. Use HOT water with the bleach. If you do this is in a bathtub, make sure you bleach and disinfect the bathtub afterwards to kill any bacteria or parasites. Its' best to clean the box outside. Mechanical cat boxes are a breeding ground for bacteria and parasites because you cannot easily disinfect them.
Dogs are no different because they also lick their anus. If you have a pet that is stretching its' behind on your carpet, you better get that pet to a vet to get wormed. You should also steam clean, at least three times a year, your carpet. Parasites can be transmitted to carpets from shoes and animals. Never walk barefoot on carpet, especially near doors. Cats should definitely be kept away from new born and infants less than three year olds. A parent that gets that sweet little kitty for their one year old is playing Russian roulette with their child's life. Parasites can exist on the fur as well. Indoor animals should be bathed regularly just like animals, twice a month, at least! And if it is an outdoor animal that comes indoors, do not let the animal lay on furniture, you are only inviting health problems.
You may think this is taking things to an extreme, but believe me, these deadly little parasites are on those dear loving pets of ours. If you own a cat, keep in strictly indoors, never let it go outdoors. If you practice these recommendations, you will find you will have less health problems. Do not under any circumstance; give your pet raw meat of any kind. You are providing the means for a parasite infection in the pet which can easily be transmitted to humans, especially children. Do not let your children play in areas where animals have defecated without spraying the area with bleach.
Animal feces should be picked up using a shovel daily and gloves should always be worn and hands washed thoroughly after any yard work. Wear a air filter mask while you do this if they area is dusty. The dust you breathe in will contain parasites. By the way, any garden work, always wear gloves. There are over 100 different parasites in soil that can be transmitted from the soil. Never work in soil if you have a cut on your hands. The little critters will get into your bloodstream via the cut. Do not flush cat box liter down the toilet. The parasites can cling to the bowl and crawl up to the seat. Once on the seat, they find their way into you. If you see rice like particles coming out in animal feces, they have worms or parasites.
Fleas are carriers of tapeworms. Recently a woman in New Jersey had severe lower colon pains and severe bloating. This went on for several months. She had two dogs in her house that she let outside every day. Several months after trying to cope with the colon pains, she then developed rashes and itching. Nine months later, they found through exploratory surgery, a large 3 and 1/2 foot tape worm inside her and several smaller ones. Upon investigation at her house, fleas were found in the carpet. Do not walk barefoot around animals unless they are strictly an indoor animal.
Tuesday, November 11, 2008
Alzheimer's disease New Look
What is dementia?
Dementia is a syndrome characterized by:
· impairment in memory,
· impairment in another area of thinking such as the ability to organize thoughts and reason, the ability to use language, or the ability to see accurately the visual world (not because of eye disease), and these impairments are severe enough to cause a decline in the patient's usual level of functioning.
Although some kinds of memory loss are normal parts of aging, the changes due to aging are not severe enough to interfere with the level of function. Many different diseases can cause dementia but Alzheimer's disease is by far the most common cause for dementia in the United States and in most countries in the world.
What is Alzheimer's disease?
Alzheimer's disease (AD) is a slowly progressive disease of the brain that is characterized by impairment of memory and eventually by disturbances in reasoning, planning, language, and perception. Many scientists believe that Alzheimer's disease results from an increase in the production or accumulation of a specific protein (beta-amyloid protein) in the brain that leads to nerve cell death.
The likelihood of having Alzheimer's disease increases substantially after the age of 70 and may affect around 50% of persons over the age of 85. Nonetheless, Alzheimer's disease is not a normal part of aging and is not something that inevitably happens in later life. For example, many people live to over 100 years of age and never develop Alzheimer's disease.
Who develops Alzheimer's disease?
The main risk factor for Alzheimer's disease is increased age. As a population ages, the frequency of Alzheimer's disease continues to increase. Ten percent of people over 65 years of age and 50% of those over 85 years of age have Alzheimer's disease. Unless new treatments are developed to decrease the likelihood of developing Alzheimer's disease, the number of individuals with Alzheimer's disease in the United States is expected to be 14 million by the year 2050.
There are also genetic risk factors for Alzheimer's disease. Most patients develop Alzheimer's disease after age 70. However, 2%-5% of patients develop the disease in the fourth or fifth decade of life (40s or 50s). At least half of these early onset patients have inherited gene mutations associated with their Alzheimer's disease. Moreover, the children of a patient with early onset Alzheimer's disease who has one of these gene mutations has a 50% risk of developing Alzheimer's disease.
There is also a genetic risk for late onset cases. A relatively common form of a gene located on chromosome 19 is associated with late onset Alzheimer's disease. In the majority of Alzheimer's disease cases, however, no specific genetic risks have yet been identified.
Other risk factors for Alzheimer's disease include high blood pressure (hypertension), coronary arteries disease, diabetes, and possibly elevated blood cholesterol.
Individuals who have completed less than eight years of education also have an increased risk for Alzheimer's disease. These factors increase the risk of Alzheimer's disease, but by no means do they mean that Alzheimer's disease is inevitable in persons with these factors.
All patients with Down syndrome will develop the brain changes of Alzheimer's disease by 40 years of age. This fact was also a clue to the "amyloid hypothesis of Alzheimer's disease" What are the symptoms of Alzheimer's disease?
What are the symptoms of Alzheimer's disease?
The onset of Alzheimer's disease is usually gradual, and it is slowly progressive. Memory problems that family members initially dismiss as "a normal part of aging" are in retrospect noted by the family to be the first stages of Alzheimer's disease. When memory and other problems with thinking start to consistently affect the usual level of functioning; families begin to suspect that something more than "normal aging" is going on.
Problems of memory, particularly for recent events (short-term memory) are common early in the course of Alzheimer's disease. For example, the individual may, on repeated occasions, forget to turn off an iron or fail to recall which of the morning's medicines were taken. Mild personality changes, such as less spontaneity, apathy, and a tendency to withdraw from social interactions, may occur early in the illness.
As the disease progresses, problems in abstract thinking and in other intellectual functions develop. The person may begin to have trouble with figures when working on bills, with understanding what is being read, or with organizing the day's work. Further disturbances in behavior and appearance may also be seen at this point, such as agitation, irritability, quarrelsomeness, and a diminishing ability to dress appropriately.
Later in the course of the disorder, affected individuals may become confused or disoriented about what month or year it is, be unable to describe accurately where they live, or be unable to name a place being visited. Eventually, patients may wander, be unable to engage in conversation, erratic in mood, uncooperative, and lose bladder and bowel control. In late stages of the disease, persons may become totally incapable of caring for themselves. Death can then follow, perhaps from pneumonia or some other problem that occurs in severely deteriorated states of health. Those who develop the disorder later in life more often die from other illnesses (such as heart disease) rather than as a consequence of Alzheimer's disease.

Ten warning signs of Alzheimer's disease
The Alzheimer's Association has developed the following list of warning signs that include common symptoms of Alzheimer's disease. Individuals who exhibit several of these symptoms should see a physician for a complete evaluation.
1. Memory loss
2. Difficulty performing familiar tasks
3. Problems with language
4. Disorientation to time and place
5. Poor or decreased judgment
6. Problems with abstract thinking
7. Misplacing things
8. Changes in mood or behavior
9. Changes in personality
10 Loss of initiative
It is normal for certain kinds of memory, such as the ability to remember lists of words, to decline with normal aging. In fact, normal individuals 50 years of age will recall only about 60% as many items on some kinds of memory tests as individuals 20 years of age. Furthermore, everyone forgets, and every 20 year old is well aware of multiple times he or she couldn't think of an answer on a test that he or she once knew. Almost no 20 year old worries when he/she forgets something, that he/she has the 'early stages of Alzheimer's disease,' whereas an individual 50 or 60 years of age with a few memory lapses may worry that they have the 'early stages of Alzheimer's disease.'
Please whatch the following sites
http://www.youtube.com/watch?v=Z6lA1P2tF0o
http://www.youtube.com/watch?v=1aXINAlMCPg&feature=related
http://www.youtube.com/watch?v=7-P9lbTJ9Hw&feature=related
Mild cognitive impairment
The criteria for dementia are conservative meaning that a patient must have had considerable decline in the ability to think before a diagnosis of dementia is appropriate. The progression of Alzheimer's disease is so insidious and slow that patients go through a period of decline where their memory is clearly worse than its baseline, yet they still do not meet criteria for dementia. This transitional syndrome is called Mild Cognitive Impairment (MCI).
Individuals affected with MCI have cognitive impairment that is demonstrated on formal neuropsychological testing but are still able to function well. Formal neuropsychological testing usually means that the patient is administered a battery of standardized tests of memory and thinking. Some of these tests are something like the IQ tests we may have taken in school. When these tests were developed they were administered to hundreds or thousands of people so that statistics are available to say how a person's score compares to a sample of healthy persons of the same age. If a person scores in the top 50%, it means that he or she did better than at least 50% of other normal people who took the test. Persons with lower scores - often in the bottom 7% - are considered to have MCI.
There are several forms of MCI. Perhaps the most common is associated with impairment in memory but not in the ability to plan and reason. Persons with this type called "amnestic MCI" (amnestic comes from "amnesia" and means no memory) have a high risk of developing Alzheimer's disease over the next few years. Persons with preserved memory but impaired reasoning or impaired judgment (call non-amnestic MCI) have a lower risk of developing Alzheimer's disease.
As treatments are developed that decrease the risk of developing Alzheimer's disease or slow its rate of progression (as of June 2007, no such medication has been approved by the FDA), recognition of amnestic MCI will be increasingly important. It is hoped that medications will be developed that will slow the rate of progression of MCI to Alzheimer's disease or completely prevent the development of Alzheimer's disease.

What are causes of Alzheimer's disease?
The cause(s) of Alzheimer's disease is (are) not known. The "amyloid cascade hypothesis" is the most widely discussed and researched hypothesis about the cause of Alzheimer's disease. The strongest data supporting the amyloid cascade hypothesis comes from the study of early-onset inherited (genetic) Alzheimer's disease. Mutations associated with Alzheimer's disease have been found in about half of the patients with early-onset disease. In all of these patients, the mutation leads to excess production in the brain of a specific form of a small protein fragment called ABeta (Aβ).
Many scientists believe that in the majority of sporadic (for example, non-inherited) cases of Alzheimer's disease (these make up the vast majority of all cases of Alzheimer's disease) there is too little removal of this Aβ protein rather than too much production. In any case, much of the research in finding ways to prevent or slow down Alzheimer's disease has focused on ways to decrease the amount of Aβ in the brain.
What are risk factors for Alzheimer's disease?
The biggest risk factor for Alzheimer's disease is increased age. The likelihood of developing Alzheimer's disease doubles every 5.5 years from 65 to 85 years of age. Whereas only 1%-2% of individuals 70 years of age have Alzheimer's disease, in some studies around 40% of individuals 85 years of age have Alzheimer's disease. Nonetheless, at least half of people who live past the 95 years of age do not have Alzheimer's disease.
Common forms of certain genes increase the risk of developing Alzheimer's disease, but do not invariably cause Alzheimer's disease. This means that in majority of patients with Alzheimer's disease, no genetic risk factor has yet been found. When medical treatments that prevent or decrease the risk of developing Alzheimer's disease become available, genetic testing may be recommended for adult children of patients with Alzheimer's disease so that they may be treated.
Many, but not all, studies have found that women have a higher risk for Alzheimer's disease than men. It is certainly true that women live longer than men, but age alone does not seem to explain the increased frequency in women. The apparent increased frequency of Alzheimer's disease in women has led to considerable research about the role of estrogen in Alzheimer's disease. Recent studies suggest that estrogen should not be prescribed to post-menopausal women for the purpose of decreasing the risk of Alzheimer's disease. Nonetheless, the role of estrogen in Alzheimer's disease remains an area of research focus.
Some studies have found that Alzheimer's disease occurs more often among people who suffered significant traumatic head injuries earlier in life, particularly among those with the apoE 4 gene.
In addition, many, but not all studies, have demonstrated that persons with limited formal education - usually less than eight years - are at increased risk for Alzheimer's disease. It is not known whether this reflects a decreased "cognitive reserve" or other factors associated with a lower educational level.

How is the diagnosis of Alzheimer's disease made?
As of June 2007, there is no specific "blood test" or imaging test that is used for the diagnosis of Alzheimer's disease. Alzheimer's disease is diagnosed when:
1) a person has sufficient cognitive decline to meet criteria for dementia;
2) the clinical course is consistent with that of Alzheimer's disease;
3) no other brain diseases or other processes are better explanations for the dementia.
What other conditions should be screened for?
There are many conditions that can cause dementia, to include the following:
Neurological disorders: Parkinson’s disease, cerebrovascular disease and strokes, brain tumors,blood clots, and multiple sclerosis, can sometimes be associated with dementia although many patients with these conditions are cognitively normal.
Infectious diseases: Some brain infections such as chronic syphilis, chronic HIV, or chronic fungal meningitis can cause dementia.
Side effects of medications: Many medicines can cause cognitive impairment, especially in elderly patients. Perhaps the most frequent offenders are drugs used to control bladder urgency and incontinence.
Psychiatric medications: such as anti-depressants and anti-anxiety medications and "neurological medications" such as anti-seizure medications can also be associated with cognitive impairment.
If a physician evaluates a person with cognitive impairment who is on one of these medications, the medication is often gently tapered and/or discontinued to determine whether it might be the cause of the cognitive impairment. If it is clear that the cognitive impairment preceded the use of these medications, such tapering may not be necessary. On the other hand, "psychiatric," "neurological," and "incontinence" medications are often appropriately prescribed to patients with Alzheimer's disease. Such patients need to be followed carefully to determine whether these medications cause any worsening of cognition.
Psychiatric disorders: In older persons, some forms of depression can cause problems with memory and concentration that initially may be indistinguishable from the early symptoms of Alzheimer's disease. Sometimes, these conditions, referred to as pseudodementia, can be reversed. Studies have shown that persons with depression and coexistent cognitive (thinking, memory) impairment are highly likely to have an underlying dementia when followed for several years.
Substance Abuse: Abuse of legal and/or illegal drugs and alcohol abuse is often associated with cognitive impairment.
Metabolic Disorders: Thyroid dysfunction, some steroid disorders, and nutritional deficiencies such as vitamin B12 deficiency or thiamine deficiency are sometimes associated with cognitive impairment.
Trauma: Significant head injuries with brain contusions may cause dementia. Blood clots around the outside of the brain (subdural hematomas) may also be associated with dementia.
Toxic Factors: Long term consequences of acute carbon monoxide poisoning can lead to an encephalopathy with dementia. In some rare cases, heavy metal poisoning can be associated with dementia.
Tumors: Many primary and metastatic brain tumors can cause dementia. However, many patients with brain tumors have no or little cognitive impairment associated with the tumor.

The Importance of Comprehensive Clinical Evaluation
Because many other disorders can be confused with Alzheimer's disease, a comprehensive clinical evaluation is essential in arriving at a correct diagnosis. Such an assessment should include at least three major components; 1) a thorough general medical workup, 2) a neurological examination including testing of memory and other functions of thinking , and 3) a psychiatric evaluation to assess mood, anxiety, and clarity of thought.
Such an evaluation takes time - usually at least an hour. In the United States healthcare system, neurologists, psychiatrists, or geriatricians, or frequently become involved. Nonetheless, any physician may be able to perform a thorough evaluation.
The American Academy of Neurology has published guidelines that include imaging of the brain in the initial evaluation of patients with dementia. These studies are either a noncontrast CT scan or an MRI scan. Other imaging procedures that look at the function of the brain (functional neuro-imaging), such as SPCT,PET and fMRI, may be helpful in specific cases, but generally are not needed. However, in many healthcare systems outside of the United States, brain imaging as not a standard part of the assessment for possible Alzheimer's disease.
Despite many attempts, identification of a blood test to diagnose Alzheimer's disease has remained elusive. As of June 2007, such testing is neither widely available nor recommended.
What is the prognosis for a person with Alzheimer's disease?
Alzheimer's disease is invariably progressive. Different studies have stated that Alzheimer's disease progresses over two to 25 years with most patients in the eight to 15 year range. Nonetheless, defining when Alzheimer's disease starts, particularly in retrospect, can be very difficult. Patients usually don't die directly from Alzheimer's disease. They die because they have difficulty swallowing or walking and these changes make overwhelming infections, such as pneumonia, much more likely.
Most persons with Alzheimer's disease can remain at home as long as some assistance is provided by others as the disease progresses. Moreover, throughout much of the course of the illness, individuals maintain the capacity for giving and receiving love, sharing warm interpersonal relationships, and participating in a variety of meaningful activities with family and friends.
A person with Alzheimer's disease may no longer be able to do math but still may be able to read a magazine with pleasure. Playing the piano might become too stressful in the face of increasing mistakes, but singing along with others may still be satisfying. The chessboard may have to be put away, but playing tennis may still be enjoyable. Thus, despite the many exasperating moments in the lives of patients with Alzheimer's disease and their families, many opportunities remain for positive interactions. Challenge, frustration, closeness, anger, warmth, sadness, and satisfaction may all be experienced by those who work to help the person with Alzheimer's disease.
The reaction of a patient with Alzheimer's disease to the illness and his or her capacity to cope with it also vary, and may depend on such factors as lifelong personality patterns and the nature and severity of stress in the immediate environment. Depression, severe uneasiness, paranoia, or delusions may accompany or result from the disease, but these conditions can often be improved by appropriate treatments. Although there is no cure for Alzheimer's disease, treatments are available to alleviate many of the symptoms that cause suffering.
 What treatment and management options are available for Alzheimer's disease?
What treatment and management options are available for Alzheimer's disease?The management of Alzheimer's disease consists of medication based and non-medication based treatments. Two different classes of pharmaceuticals are approved by the FDA for treating Alzheimer's disease: cholinesterase inhibitors and partial glutamate antagonists. Neither class of drugs has been proven to slow the rate of progression of Alzheimer's disease. Nonetheless, many clinical trials suggest that these medications are superior to placebos (sugar pills) in relieving some symptoms.
Cholinesterase inhibitors
In patients with Alzheimer's disease there is a relative lack of a brain chemical neurotransmitter called acetylcholine. (Neurotransmitters are chemical messengers produced by nerves that the nerves use to communicate with each other in order to carry out their functions.) Substantial research has demonstrated that acetylcholine is important in the ability to form new memories. The cholinesterase inhibitors (ChEIs) block the breakdown of acetylcholine. As a result, more acetylcholine is available in the brain, and it may become easier to form new memories.
Four ChEIs have been approved by the FDA, but only donepezil hydrochloride (Aricept), rivastigmine (Exelon), and galatamine (Razadyne - previously called Reminyl) are used by most physicians because the fourth drug, tacrine (Cognex) has more undesirable side effects than the other three.
Most experts in Alzheimer's disease do not believe there is an important difference in the effectiveness of these three drugs. Several studies suggest that the progression of symptoms of patients on these drugs seems to plateau for six to 12 months, but inevitably progression then begins again.
Of the three widely used AchEs, rivastigmine and galantamine are only approved by the FDA for mild to moderate Alzheimer's disease, whereas donepezil is approved for mild, moderate, and severe Alzheimer's disease. It is not known whether rivastigmine and galantamine are also effective in severe Alzheimer's disease, although there does not appear to be any good reason why they shouldn't.
The principal side effects of ChEIs involve the gastrointestinal system and include nausea, vomiting, cramping, and diarrhea. Usually these side effects can be controlled with change in size or timing of the dose or administering the medications with a small amount of food. Between 75% and 90% of patients will tolerate therapeutic doses of ChEIs.
Partial glutamate antagonists
Glutamate is the major excitatory neurotransmitter in the brain. One theory suggests that too much glutamate may be bad for the brain and cause deterioration of nerve cells. Memantine (Namenda) works by partially decreasing the effect of glutamate to activate nerve cells. It has not been proven that memantine slows down the rate of progression of Alzheimer's disease. Studies have demonstrated that some patients on memantine can care for themselves better than patients on sugar pills (placebos). Memantine is approved for treatment of moderate and severe dementia, and studies did not show it was helpful in mild dementia. It is also possible to treat patients with both AchEs and memantine without loss of effectiveness of either medication or an increase in side effects.
Non-medication based treatments
Non-medication based treatments include maximizing patients' opportunities for social interaction and participating in activities such as walking, singing, dancing that they can still enjoy. Cognitive rehabilitation, (whereby a patient practices on a computer program for training memory), may or may not be of benefit. Further studies of this method are needed.
 Treatment of psychiatric symptoms
Treatment of psychiatric symptomsSymptoms of Alzheimer's disease include agitation, depression, hallucinations, anxiety, and sleep disorders. Standard psychiatric drugs are widely used to treat these symptoms although none of these drugs have been specifically approved by the FDA for treating these symptoms in patients with Alzheimer's disease. If these behaviors are infrequent or mild, they often do not require treatment with medication. Non-pharmacologic measures can be very useful.
Nevertheless, frequently these symptoms are so severe that it becomes impossible for caregivers to take care of the patient, and treatment with medication to control these symptoms becomes necessary. Agitation is common, particularly in middle and later stages of Alzheimer's disease. Many different classes of agents have been tried to treat agitation including:
antipsychotics,
Mood-stabilizing anticonvulsants,
. Trazodone (Desyrel)
. Anxiolytics
. Beta–blockers.
Studies are conflicting about the usefulness of these different drug classes. It was thought that newer, atypical antipsychotic agents such as clozapine (Clozaril), risperidone (Risperdal), olanzapine (Zyprexa, Zydis), quetiapine (Seroquel), and ziprasidone (Geodon) might have advantages over the older antipsychotic agents because of their fewer and less severe side effects and the patients' ability to tolerate them. However, more recent studies have not demonstrated superiority of the newer antipsychotics. Some research shows that these newer antipsychotics may be associated with increased risk of stroke or sudden death than the older antipsychotics, but many physicians believe this question is still not resolved.
Apathy and difficulty concentrating occur in most Alzheimer's disease patients and should not be treated with antidepressant medications. However, many Alzheimer's disease patients have other symptoms of depression including sustained feelings of unhappiness and/or inability to enjoy their usual activities. Such patients may benefit from a trial of antidepressant medication. Most physicians will try selective serotonin reuptake inhibitors (SSRIs), such as sertraline (Zoloft), citalopram (Celexa), or fluoxetine (Prozac), as first-line agents for treating depression in Alzheimer's disease.
Anxiety is another symptom in Alzheimer's disease that occasionally requires treatment. Benzodiazepines such as diazepam (Valium) or lorazepam (Ativan) may be associated with increased confusion and memory impairment. Non-benzodiazepine anxiolytics, such as buspirone (Buspar) or SSRIs, are probably preferable.
Difficulty sleeping (insomnia) occurs in many patients with Alzheimer's disease at some point in the course of their disease. Many Alzheimer's disease specialists prefer the use of sedating atypical antidepressants such as trazodone (Desyrel). However, other specialists may recommend other classes of medications. Sleep improvement measures, such as sunlight, adequate treatment of pain, and limiting nighttime fluids to prevent the need for urination, should also be implemented.
Potential and future therapies for Alzheimer's disease
A variety of clinical research trials are underway with agents that try either to decrease the amount of Aβ1-42 produced or increase the amount of Aβ1-42 removed. It is hoped that such therapies may slow down the rate of progression of Alzheimer's disease. As of June 2007, it is not known how well such therapies may work.
Caring for the caregiver and Alzheimer's disease resources
Caring for the caregiver is an essential element of managing the patient with
Alzheimer's disease. Caregiving is a distressing experience. On the other hand, caregiver education delays nursing home placement of Alzheimer's disease patients. The 3Rs - Repeat, Reassure, and Redirect - can help caregivers reduce troublesome behaviors and limit the use of medications. The short-term educational programs are well liked by family caregivers and can lead to a modest increase in disease knowledge and greater confidence among caregivers.
Alzheimer's Disease At A Glance
Alzheimer's disease is a brain disease of unknown cause that leads to dementia.
Most patients with Alzheimer's disease are over 65 years of age.
 One of Hollywood's most iconic stars, Charlton Heston, has died at age 84. His death was not unexpected. Heston had been suffering from the ravages of advanced Alzheimer's Disease since 2002
One of Hollywood's most iconic stars, Charlton Heston, has died at age 84. His death was not unexpected. Heston had been suffering from the ravages of advanced Alzheimer's Disease since 2002· memory loss,
· difficulty performing familiar tasks,
· problems with language,
· disorientation to time and place,
· poor or decreased judgment,
· problems with abstract thinking,
· misplacing things,
· changes in mood or behavior,
· changes in personality,
· loss of initiative.
Patients with symptoms of dementia should be thoroughly evaluated before they become inappropriately or negligently labeled Alzheimer's disease. Although there is no cure for Alzheimer's disease, treatments are available to alleviate many of the symptoms that cause suffering.
The management of Alzheimer's disease consists of medication based and non-medication based treatments organized to care for the patient and family.
Treatments aimed at changing the underlying course of the disease (delaying or reversing the progression) have so far been largely unsuccessful. Medicines that restore the defect, or malfunctioning, in the chemical messengers of the nerve cells have been shown to improve symptoms.
Herbal products can help maintain the life of Alzheimer’s patients
· Huperzine, an anticholinesterase alkaloid, is divided into two chemical species, huperzine A and huperzine B, which have similar effects but differing activity levels (huperzine A being about 10 times as strong as huperzine B).
· Macleaya cordata
· Coptis chinenses
· Securinega suffruticosa
· Pinus pinaster ssp
· Ginkgo biloba 120 to 240 mg a day
· Rosemary
· Lecithi
· angelica or dong-quai·
· American Ginseng
Supplements.
· Vitamin E 2,000 IU
· Acetyl-L-carnitine 1,500 mg a day
· Phenylalanine
· S-Adenosylmethionine (SAMe)
· Tyrosine Vitamin C (Ascorbic Acid)
· Vitamin A (Retinol)
· Vitamin B1 (Thiamine)
· Vitamin B12 (Cobalamin)
· Vitamin B9 (Folic Acid)
Sites of interest:
http://www.xcell-center.com/
http://www.stammzellendokumentation.de/engl.html
Thursday, November 6, 2008
Parkinson's disease, full spectrum information
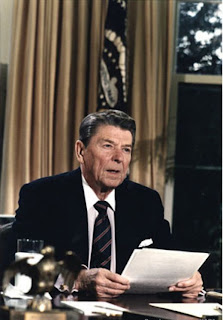
 Two well know celebrity, suffering from Parkinson’s disease
Two well know celebrity, suffering from Parkinson’s diseaseParkinson's disease is named after the English physician Dr. James Parkinson, who described it in 1817. However there is a much earlier description of Parkinson's disease among the writings of Leonardo da Vinci, in the Royal collection at Windsor Castle in England.Parkinson's disease (PD) is a slowly progressive condition resulting from a deficiency in the brain of a chemical called dopamineDopamine is one of many chemical messengers (called neurotransmitters) in the brain that allow nerve cells to communicate with each other. Without it, messages from the brain to the muscles are disrupted.
Over a period of time symptoms appear that include:
.Tremor (shaking) when the body and limbs are at rest
.Slowness and difficulty beginning a voluntary movement, such as standing up from a chair or turning around, and difficulty with fine precise movements such as doing up buttons. (called bradykinesia).
.Muscle stiffness, also called rigidity, and Difficulty with maintaining balance (called postural instability)
The amount of dopamine in the brain is reduced in Parkinson's disease because some of the nerve cells that produce it are destroyed.The small group of nerve cells affected in Parkinson's disease nerve cells lies deep in the brain, in a region called the substantia nigra or (black substance), a part of the brain involved in initiating movement. It is situated near the center of the brain and contains a clump of dark cells that manufacture dopamine
Facts About Parkinson's Disease·
The incidence of Parkinson's disease is increasing at a rate that is faster than the population is aging.· Parkinson's disease affects an estimated 1 in 1,000 people over age 55.· Parkinson's disease affects about 1 in 100 people age 65 and older.· Some 20 percent of people with Parkinson's disease may be diagnosed under the age of 50.· About 8 percent to 10 percent of people with Parkinson's disease may be diagnosed under the age of 40.
Well-known people who have had or have Parkinson's disease include Pope John Paul II, Francisco Franco, Muhammad Ali, Yasir Arafat, Janet Reno, Sir Michael Redgrave, Adolf Hitler, Vincent Price, Morris Udall, Margaret Bourke White, Pierre Elliot Trudeau, and Michael J. Fox.·
There has been excellent progress with research into the treatment of Parkinson's disease. This includes stem cell technology in which very basic cells are grown in the laboratory, and can be easily cultivated into large populations. Researchers have succeeded in turning these stem cells, in the laboratory, into dopamine producing nerve cells, like those cells in the substantia nigra of the brain that produce dopamine.· Human trials have already begun and been published using retinal epithelial cells, and human trials using stem cells for the treatment of Parkinson's disease should begin in the foreseeable future.What Causes Parkinson's Disease ?Deep inside the brain, in an area of the brain called the basal ganglia, are nerve cells that normally control a person's voluntary movement and coordinate changes in person’s posture.

Basal ganglia and substantia nigra
When the brain sets in motion an action that results in lifting an arm, for instance, the basal ganglia signals and transmits messages to the other parts of the brain.Those messages are forwarded as electrical impulses along and between nerve pathways by the chemical messenger called dopamine, which is made in the area of the brain called the substantia nigra. The message passes on to the basal ganglia and down the spinal cord to the muscles used to lift the arm.The basal ganglia are normally rich with this chemical called dopamine which has been delivered from a nearby area in the brain called the substantia nigra where the dopamine is manufactured.· In people with Parkinson's, the nerve cells in the substantia nigra (where the dopamine is made) die, and the surviving cells do not produce enough dopamine.·
The symptoms of Parkinson's will begin when 80 percent of dopamine production from this area of the brain is lost. We do not know why some previously normal nerve cells die causing dopamine levels to fall.
· Parkinson's is known to occur in some families, (10 percent to 15 percent of Parkinson's disease may be inherited) and several genes, have been identified in the last decade that appear to be associated with Parkinson's and undoubtedly more will be discovered as research continues. However, not all familial Parkinson's disease is inherited and in these cases it may occur as a result of a shared environment and a common susceptibility.
· When Parkinson's disease is inherited, it tends to occur in people under fifty years of age. However, this does not mean that everyone who develops Parkinson's under the age of fifty has inherited the disease.
· The majority of people with have what is called sporadic disease, which means it occurs in the absence of a family history with no known cause.· Researchers feel that there may be more than one
cause of disease.
· There is renewed interest in the possibility that a virus might be one cause of Parkinson's. Parkinson's was a complication of the influenza pandemic that occurred after World War 1. This virus disappeared in the early 1930s, before it could be identified. Animal studies support this, and two studies in humans showed that Parkinson's is much more common in people who work and live in close contact with others.
· The most recent study involved confirmed earlier findings that teachers and members of the medical profession carry twice the risk. The last study found no increase in Parkinson's in welders.
· A recent study described three statistically significant clusters of people who worked together and who developed Parkinson’s within a similar time frame. One involved 4 members of a TV cast and crew (4 subjects out of 120) one a group of professors (4 subjects out of 30) and one a group of people in the office of a garment factory (3 out of 7). The authors do not speculate on the cause but each group worked in an environment with artificial ventilation.
· There are still some scientists who think that "free radicals" may contribute to the damage to the nerve cells. These are toxic substances made in the body as a result of normal chemical reactions. Some people with Parkinson’s have increased levels of iron in the brain, which is part of the oxidation process. The implication of these findings is unclear.
· Aluminum toxicity. Aluminum is one of the most abundant minerals found on earth,and one of the most toxic to humans. Aluminum damages nervous systems in both infants and adults. It is implicated in anemia, osteomalacia, glucose intolerance, memory deficits, and Alzheimer's, Lou Gehrig's (amyotrophic lateral sclerosis), and Parkinson's diseases. Scientists do not yet understand whether aluminum is a primary cause of Alzheimer's or is accumulated in the brain as a result of a malfunction caused by the disease. They do know, however, that aluminum wreaks havoc on human nervous systems and should be avoided.
· In some cases, the cause is known. Parkinsonism can be a consequence of some medications (used to treat psychiatric illness or control nausea). A small group of people developed Parkinsonism as a result of a known toxin called MPTP, found in an illegal synthetic opiate-derivative street drug and sold in California in the early 1980s.
What Are The Signs And Symptoms Of Parkinson's Disease?
Parkinson's disease has classic signs and symptoms, but they do not all appear at the same time or to the same degree. Some people are more troubled by one than another. The condition can vary significantly between individuals, for example how the disease progresses, and how well someone responds to the drugs, etc. Therefore, people with PD should never compare themselves with others who have PD.

Parkinson captivity on wheelchair
These Are The Four Major Signs Of PD:
Tremor.
In about 70 percent of people with PD, this is the earliest symptom to appear. It is a tremor that occurs in a limb when it is at rest. The tremor starts in one arm or leg on one side of the body and can progress to include the other side of the body. It usually remains more pronounced on one side of the body. Although socially distressing, the tremor does not usually interfere with activities of daily life, and it tends to disappear with voluntary movement (picking up a cup, for example). Often, medications do not completely control tremor. Fatigue, emotional stress, and worrying about the tremor can make it worse in the short term.
Rigidity.
This describes increased tone or stiffness in the muscles when they are at rest. Joints may sometimes feel locked. The lack of mobility often causes muscle fatigue and ache. Rigidity usually responds well to treatment.Slowness of movement. This condition is called bradykinesia. Fine movements become clumsy, for example, doing up buttons. Typically, it is often hard to begin a movement, for example, getting up from a chair, or there may be an abrupt stopping of ongoing movement such as when turning corners or going through doorways. This symptom is the most disabling, but it responds well to treatment.
Impaired balance.
Normally, reflexes allow us to make rapid adjustments to changes in the body's center of gravity when standing or walking. These reflexes become impaired in people with PD who may eventually be at risk for falls. Medication may help, but rehabilitation therapy is most valuable.Symptoms:There are also a number of symptoms associated with PD. Not all people will experience them to the same degree.
They include:
A changed facial expression.Because the facial muscles that normally create expression don't move as well, people with PD sometimes appear to look uninterested or sad when they are not. This is known as hypomimia.A soft voice.This is known as hypophonia. People with PD may have difficulty being heard, particularly on the phone.
In addition, the rhythm of the voice can be affected, and words may be spoken in a monotone.Small, cramped handwriting.Writing may be normal size for the first few words and then will trail off and get smaller. This is known as micrographia.Pain.Painful stiffness, for example affecting the shoulder or calves, is a common early feature of PD. Painful cramps can also affect some people, sometimes as a result of too much medication and sometimes too little. The physician will want to know when the cramps occur in relationship to the timing of the drugs.
Successful treatment of PD symptoms can lead to improved mobility, but can sometimes aggravate existing arthritis.Fatigue.Everyday tasks take longer to complete when one has PD. It is hard to do two things at once. Sleep may also be disturbed. When combined, these problems often contribute to the tiredness experienced by many. It also takes a while for people with PD to learn to pace themselves to avoid reaching the end of a day without feeling exhausted. Some people experience a noticable benefit in their symptoms after a good nap or a sleep.Depression.Research indicates that up to 50 percent of patients with PD can experience a period of depression during their illness.
Depression in PD is caused by disturbed brain chemistry, and it can be triggered or made worse by stressful situations in life. Depression may occur at any time during the illness. But if depression is present when the person is first diagnosed with PD, it sometimes gets better on its own when PD symptoms start to improve with treatment.Depression may, however, need some treatment itself. The most important first step is for the person with PD to be able to admit to being depressed and seek appropriate help. Today's antidepressants are safe and well tolerated, and most can be taken very successfully with antiparkinson drug therapy. There may be mild side effects early in treatment (dry mouth, dizziness, drowsiness), but these usually disappear with time.
Full benefit from treatment for depression can take from four to six weeks. Patience, determination, and family support are needed while the right dose level is achieved.Constipation.PD and the drugs used for its treatment contribute to constipation. Severe constipation can lead to a medical emergency. If constipation continues to be a problem, it is important to seek medical help.
Intellectually, people with PD usually remain normal. But because speech and everyday tasks take longer to execute, it may appear that they lack comprehension or understanding - when actually they know exactly what they want to do but are unable to process their thoughts or actions in a timely manner. Some 30 percent of patients with PD, however, do develop dementia - the loss of cognitive and intellectual functions without impairment of perception or consciousness. Dementia can also lead to disorientation, a flattened mood, impaired memory, judgment, and intellect.
Medications Used to Treat Parkinson's Disease

Nice To Know:
A few important comments before describing the medications for Parkinson's DiseaseDrug therapy for Parkinson's disease, and the choice of drugs used for the treatment of Parkinson's disease, should be a joint decision between the person with Parkinson's disease and the physician, based on the severity of symptoms and their impact on quality of life.
· It is emphasized that treatment for Parkinson's disease should always be individually tailored for each person.
· Never compare your treatment schedules with those of other people with Parkinson's Disease. You are all different.
· Properly selected medications with the correctly tailored dose form the mainstay of treatment of Parkinson's Disease.Drugs currently used to treat Parkinson's Disease make movement easier and can prolong function for many years.
Medications aim to replace or mimic the missing chemical dopamine, in the brain.The following are the medications used in the treatment of Parkinson's Disease. Each will be considered below.
1- Levodopa with carbidopa:
SinemetTMSinemet CRTM Levodopa, with benserazide,:
2- ProlopaTM in Canada and MadoparTM in Europe
3- COMT inhibitors:entacapone (ComtanTM), TasmarTM)
Dopamine agonists:
pramipexole,MirapexTM), ropinerole ( RequipTM), bromocriptine( ParlodelTM), pergolide ( PermaxTM)
Other medications:amantadine (SymmetrelTM), benztropine (CogentinTM), trihexyphenydil (ArtaneTM), deprenyl (EldeprylTM) Levodopa

Carbidopa or benzerazide prevent levodopa from being converted to dopamine outside the brain.They allow more levodopa to enter the brain where it is needed.They help to reduce or prevent the side effects of dizziness and nausea.The combination is usually started with low, but increasing doses, until the best effect is achieved.
Sinemet CRTM (controlled-release drug)· 200/50 peach oval scored· 100/25 pink oval
Sinemet CRTM is a controlled-release tablet of levodopa/carbidopa.


The improvements were evident at a checkup three months after the procedure and persisted to the end of the study, one year after the surgery, researchers reported. By that time, the overall amount of improvement from before surgery was about 24 percent when measured at times that patients were off their normal medication, and 27 percent at times when they were on medication.
After some surgical procedures (for e.g. abdominal surgery) you will not be able to take anything by mouth.If this is the case you should ask about having a nasogastric tube inserted before surgery even if the surgeon does not usually insert one for your procedure. You must be able to restart your anti-Parkinson drugs as soon as possible post-operatively to ensure optimal mobility. Post-surgery, crushed regular levodopa can be given with water through tube. Other tablets and the contents of capsules can be administered via nasogastric tube. However, Sinemet alone is preferred for the first few days to minimize the risk of psychosis and nausea.
Parkinson’s Disease is already creating stress, so your body may be less able to cope with additional problems and adapt to the hospital environment.Stress reduces energy for healing and will make all Parkinson’s Disease symptoms worse.
ConstipationIt is important to embark on a program of prevention rather than crisis management.

Great progress has already been made in three distinct realms of PD:· Increasing knowledge about the causes of PD, including the identification of four genes for PD as well as some clues to environmental causes. (PD is twice as common in people who work closely with other members of the public.)·
A: This is untrue for the majority of patients with PD. We all need adequate amounts of all the food groups to maintain health. A protein redistribution diet can be useful in a very, very small number of patients who have fluctuations in response to their standard SinemetTM. This diet should be developed with the cooperation of your dietician and neurologist. If it is not effective in one week, it should be abandoned. It is true that any extra-large meal can cause a delay in gastric emptying and this may make anyone feel sluggish and tired. Most people with PD do better eating more frequent smaller meals with high-energy, easily digestible snacks in-between.
Phenylalanine
S-Adenosylmethionine (SAMe)
Tyrosine Vitamin C (Ascorbic Acid)
Vitamin A (Retinol)
Vitamin B1 (Thiamine)
Vitamin B12 (Cobalamin)
Vitamin B9 (Folic Acid)
Vitamin E
Fava Beans, Levodopa, and Parkinson's DiseaseBy Kathrynne Holden, MS, RDMs.
Yes, there a number of concerns to be aware of:Variable levodopa amounts. Because fava plants have varying amounts of levodopa, it's possible to get either too much or too little levodopa. Too little levodopa will not relieve PD symptoms; and too much levodopa can cause overmedication effects, such as dyskinesia - particularly if other PD medications are being used at the same time. Also, the levodopa can cause nausea in some people.
Favism .. is an inherited disease in which a person lacks an enzyme called glucose-6-phosphate dehydrogenase (G6PD). When these people eat fava beans, they develop a condition called hemolytic anemia. This anemia causes red blood cells to break apart and block blood vessels. When such blockage occurs in the kidneys, it can result in kidney failure and even death. Although favism is usually detected in childhood, adults can be affected as well.G6PD deficiency is rare, occurring mostly among people of Mediterranean, African, and Southeast Asian descent, but others can be affected as well. Your physician can perform a blood test for G6PD to determine whether you are at risk. If you find you have inherited G6PD deficiency, your dietitian can help you locate other foods that may be of concern, and can help you plan safe and healthful menus. For more information on favism.
Please watch the following sites
http://www.youtube.com/watch?v=hrfAj-HUjzU&NR=1
To use the fresh green fava beans, shell the beans from the pods, like green peas. Then boil or steam them till tender - usually two to 10 minutes, depending on size and age. Add butter, salt and pepper, or your own favorite seasoning, and serve as a side dish. You can also add the cooked beans to salads. If the beans seem too chewy, cook for 8-10 minutes, then cool and slip off the outer skins; cook a few more minutes if needed. Some people like to eat the skins, others find them too tough.
In conclusion, fava beans are an excellent food, as well as a possible way to help fight the effects of PD. Discuss use of fava with your doctor and registered dietitian. Here's to your good health!































